Iron Deficiency—What you need to know
It’s a familiar story for many women… you get blood tests, your ferritin is low, and the conclusion is you’re ‘iron deficient’. The usual prescription? An iron tablet or, in more severe cases, an infusion.
It feels like the answer… but here’s the catch, it often isn’t. In fact, this approach can actually keep you stuck in the low-iron cycle.
Let’s unpack why. But first… Iron 101: Why It’s Essential
Transports oxygen in blood and muscle
Supports fatty acid metabolism
Keeps your immune system functioning
But here’s something most people don’t know… A typical diet contains approximately 10−20 mg iron/day, but the fixed-rate physiological uptake route allows for absorption of only up to 5 mg at a time. A therapeutic oral iron dose of, for example, 100 mg, thus largely exceeds the amount that can be taken up via the active absorption pathway.”
So when you pop a supplement with 70–100 mg of iron—or get an infusion of 1000–1600 mg—you’re far exceeding what your body can use. The excess doesn’t simply vanish. In fact…“There is no active excretory process for iron once it has entered the bloodstream.”
Why Supplements or Infusions may exacerbate the issue…
Evidence reveals that excess, unabsorbed iron doesn’t just sit quietly in the system. Instead, it results in undesirable side effects “at the intestinal host–microbiota interface” and can stimulate the growth of bacterial pathogens, making them more virulent and thus lead to ‘dysbiosis’ and a vicious cycle of ‘iron deficiency’.
Iron Storage in the Body…
The body has no natural method of excreting excess iron. When there’s too much, it gets stored in organs and joints. Over time, this storage can overload the liver and create other health problems such as arthritis, heart disease, diabetes, endocrine disruption, and even sexual dysfunction.
Impact on Thyroid Function…
It starts with low iron… and next on the list for so many women is disrupted thyroid function. Metabolism slows, belly gets a spare tyre and so on. The “Thyroid may be directly affected by iron storage in the gland as well as functionally altered due to iron accumulation occurring in the pituitary.”
Blood Sugar Disregulation…
Excess iron can affect the islets of Langerhans — tiny islands of endocrine cells scattered throughout the pancreas that are particularly vulnerable to iron. Accumulation here can induce oxidative damage of pancreatic beta-cells. These beta cells are the ones responsible for making insulin, the hormone that regulates blood glucose. Damage to them can lead to conditions such as hypoglycaemia or diabetes.
Pathogen Virulence…
In the gut itself, excess iron may enhance the virulence of enteric pathogens, favouring colonisation and even increasing their ability to adhere to and invade the intestinal lining.
Adversely affects the Gut …
Excess iron also alters gut microbiota composition, often leading to a decrease in beneficial families like Bifidobacteriaceae and Lactobacillaceae while increasing coliforms and E. coli. It also adversely affects the gut microbiome, increasing pathogen abundance and causing intestinal inflammation. This shift tends to increase protein fermentation, leading to the formation of toxic by-products, while at the same time interfering with beneficial carbohydrate metabolism.
Iron overload and Neurodegenerative diseases…
Research shows… “Iron accumulation are hallmarks of a variety of neurodegenerative diseases that include Parkinson’s disease (PD) and Alzheimer’s disease (AD)”
“Interestingly, the brain regions which suffered neuronal degeneration and brain atrophy were highly coincident with the sites of iron accumulation (Horvath et al., 2012), these findings strongly suggest that the excess iron accumulation is linked to interferonopathies of AD.”
The gut-food connection…
Here’s where most conversations about iron miss the mark… 🔑 Your gut microbiome is the main regulator of iron.
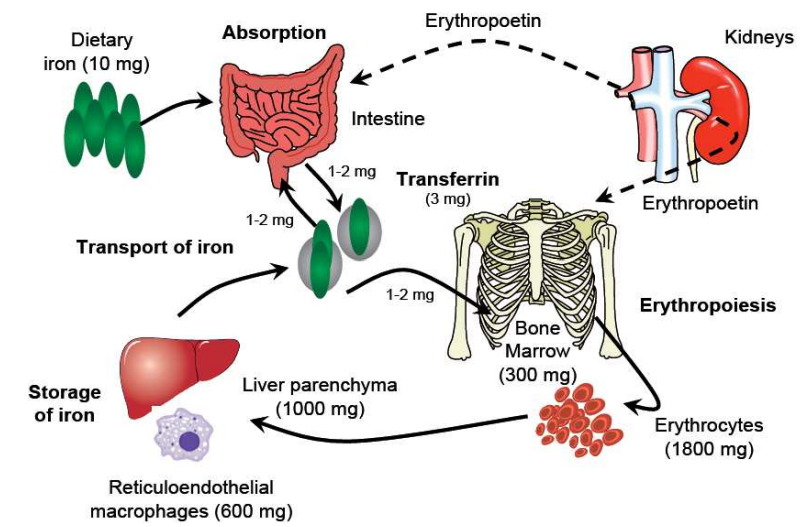
Eating ‘plants’ matters—two-thirds of the body’s iron is tied up in red blood cells produced in bone marrow. And it’s your gut microbes that sustain this process. And they NEED fibre to survive and thrive.
Key disruptors to iron absorption…
Antibiotics → strip gut microbes and inflame the gut lining
Alcohol → lowers stomach acid, inflames villi, and disrupts hepcidin (the hormone that regulates iron)
Medications (antacids, painkillers, antihistamines) → block the conversion of iron.
Over-exercise → endurance athletes lose up to 70% more iron via sweating, gut bleeding, and red cell breakdown.
Everyday Habits That Block Iron…
🚫 Tea & coffee → A single cup of tea reduces non-haem iron absorption by 75–80%, coffee by ~60%. Rooibos is a better alternative: zero tannins.
🚫 Turmeric (in excess) → binds to ferric iron, blocking absorption (20–90%).
🚫 Calcium, Magnesium & Zinc supplements → compete with iron at the absorption level. Adding cheese or milk to a meal can cut iron uptake by 50–60%.
Stress, The Hidden Driver of Iron Deficiency…
When it comes to iron deficiency, most people immediately think of diet. But research shows the main culprit is often stress — and the effects run deep.
How Stress Disrupts Iron Regulation…
Stress affects the HPA axis (the hypothalamic–pituitary–adrenocortical axis), setting off a cascade that leads to a proinflammatory state and alters hepcidin — the key hormone that regulates iron absorption. In fact, a 2023 study revealed…
“Psychological stress responses may engage similar pathways as infectious stress, which alters fundamental iron metabolism processes and cause functional tissue-level iron deficiency. Psychological stress, analogous to but to a lesser degree than infectious stress, activates the hypothalamic–pituitary–adrenocortical (HPA) axis and increases proinflammatory cytokines. Chronic or severe stress is associated with dysregulated HPA axis functioning and a proinflammatory state. This dysregulation may disrupt iron absorption and utilization, likely mediated by the IL-6 activation of hepcidin, a molecule that impedes iron absorption and redistributes total body iron.”
In short… stress literally changes the way your body handles iron, blocking absorption and shunting it away from where it’s needed.
The Impact on Serum Iron Levels…
Stress doesn’t just influence iron — it actively reduces it. Studies show that stress can decrease serum iron levels, and prolonged stress — even when it’s purely psychological — leads to significant drops in both serum iron and bone marrow iron compared with non-stressed controls. Erythropoiesis (the development of red blood cells) is also impaired. As one study highlighted… “Serum iron level was decreased after 3-days repeated psychological stress exposure before the decline of red cell count and hemoglobin.”
This means stress lowers iron before your blood counts even start to fall.
Stress and Red Blood Cell Formation…
The damage doesn’t stop there. Prolonged stress has been shown to actually inhibit the synthesis of hemoglobin (Hb) and disrupt erythropoiesis. Or as researchers put it… “Psychological Stressors lead to the decreased iron absorption and iron redistribution in body induced the decreased serum iron and bone marrow iron and inhibited the synthesis of hemoglobin (Hb) and erythropoiesis.”
The Bottom Line…
It’s not always about how much iron you eat — it’s whether your body can use it. And stress is one of the biggest barriers to healthy iron levels, quietly undermining absorption, storage, and blood cell production.
What Helps Iron Absorption?
Eating more PLANTS… cos they’re packed with fibre AND iron and are ‘naturally’ infused with Vitamin C.
Including servings of full-fat ORGANIC yoghurt, cheese and Kefir in your diet.
Altering your LIFESTYLE… addressing all the areas that bring ‘stress’ into your life!
It’s SIMPLE… these pathways restore the gut, restore your iron—and break the cycle for good.
Always Look Deeper…
If your iron is low, don’t just ‘top it up’. Look deeper. One of the first priorities is ruling out hidden blood loss. Here are the most common investigations…
Blood Tests…
Full Blood Count (FBC/CBC) → checks for anaemia and red blood cell patterns.
Iron studies (Ferritin, Transferrin Saturation, Serum Iron, TIBC) → confirm deficiency vs. poor utilisation.
Stool Occult Blood Test (FOBT or FIT test) → looks for microscopic (hidden) blood in stool.
Gastrointestinal Investigations…
Since the GI tract is the most common source of chronic hidden bleeding…
Gastroscopy (upper endoscopy) → examines oesophagus, stomach, duodenum for ulcers, gastritis, varices, or cancers.
Colonoscopy → examines the colon and rectum for polyps, inflammatory bowel disease, haemorrhoids, or cancers.
Capsule Endoscopy (if first scopes are clear) → tiny camera capsule swallowed to check the small intestine for bleeding, vascular lesions, or tumours.
Other Possible Tests…
Urinalysis → rules out blood loss through the urinary tract (e.g. kidney/bladder issues).
Pelvic Ultrasound (women) → checks for fibroids, heavy menstrual bleeding causes.
Haemolysis workup (if appropriate) → not technically “blood loss,” but excessive red blood cell breakdown can mimic iron deficiency patterns.
While it’s great you’ve read this far — I’m going to be blunt… knowledge is powerful but taking action is what leads to change. If you want to talk through what’s going on for you and get clarity as to next best steps, let’s chat👉Book a free Clarity call → here
P.S. I mostly work with women 50+, but I’ll work with women outside that age group if it’s the right fit.
With (gut) love, Nat 💚
References
Inhibitory Effect of Calcium on Non-heme Iron Absorption May Be Related to Translocation of DMT-1 at the Apical Membrane of Enterocytes. 2010.
Calcium and iron absorption: mechanism of action and nutritional importance. 1992.
Iron deficiency anemia induced by magnesium overuse: a case report. BioPsychoSocial Med. 2019.
Interactions between magnesium and iron. In vitro studies. Arzneimittelforschung. 1994.
Exercise-induced anaemia: a forgotten cause of iron deficiency anaemia in young adults. The British journal of general practice: The journal of the Royal College of General Practitioners. 2015.
Effects of psychological stress on serum iron and erythropoiesis. International Journal of Hematology. 2008.
Iron-bioavailability-of-cocoa-powder-as-determined-by-the-hb-regeneration-efficiency-method. 2008
Association between Haem and Non-Haem Iron Intake and Serum Ferritin in Healthy Young Women. 2017
Dietary intake and iron status of Australian vegetarian women. 2021.
Does calcium interfere with iron absorption. 2020
Hyperferritinemia and inflammation. 2017
Intestinal parasitic infestations and anemia. 2018
Iron and Parasites. 2015
Iron deficiency anemia induced by magnesium overuse: a case report. 2019
Iron Status of Vegetarian Adults: A Review of Literature. 2016
Lifestyle characteristics and nutrient intakes in a cohort of 33 883 meat-eaters and 31 546 non meat-eaters in the UK. 2002
Is achlorhydria a cause of iron deficiency anemia. 2015
Is Higher Consumption of Animal Flesh Foods Associated with Better Iron Status among Adults in Developed Countries? A Systematic Review. 2016.
Nutritional iron turned inside out: intestinal stress from a gut microbial perspective. 2014
Inflammation alters the expression of DMT1, FPN1 and hepcidin, and it causes iron accumulation in central nervous system cells. 2013.
Role of alcohol in the regulation of iron metabolism. 2007
The effect of psychological stress on iron absorption in rats. 2009
The Interaction between Psychological Stress and Iron Status on Early-Life Neurodevelopmental Outcomes. 2023
Ferroptosis as a mechanism of neurodegeneration in Alzheimer's disease. 2021
Ferroptosis, a Potential Therapeutic Target in Alzheimer’s Disease. 2021
Role of Oxidative Stress and Lipid Peroxidation in the Pathophysiology of NAFLD. 2022